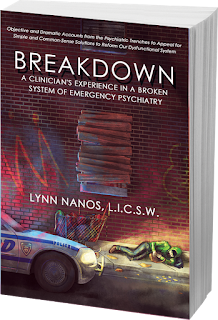
I finished reading Breakdown: A Clinician's Experience in a Broken System of Emergency Psychiatry, by Lynn Nanos. The opening page of Breakdown quotes Dorothea Dix: “…I come as the advocate of helpless, forgotten, insane, and idiotic men and women….” Like the Civil War era Dorothea, Lynn Nanos is a Massachusetts woman and tireless advocate for people with serious mental illness.
As a parent of a thirty-year participant in the mental health
system, I found Breakdown informative, comprehensive, well-researched, and thoroughly-referenced.
Practical advice and familiar vignettes weave through the narrative as only
someone who has been on the front lines of psychiatric emergencies can document.
Each of the twenty-two chapters is focused and does not shy away from difficult
issues or controversial positions. Nanos’ experiences as a clinician in
Massachusetts document the roles, laws, and regulations in that state as I ponder my state of Idaho. For instance, what is a Roger’s
Monitor in Massachusetts and how does this compare to Idaho? This is a court order for patients to receive antipsychotic medication regardless of whether they want such medication. Many people with mental illness do not adhere to treatment recommendations because they lack awareness of being ill.
Nanos tells stories of
individual crises, which she skillfully uses to document the complex problems
surrounding the personal and societal costs of mental illness. I am intrigued
by her ability to tell the stories of countless individuals from her perspective as a professional clinician in an urban setting. By
contrast, I am one family member, an artist and knitting machine educator by
trade, with one long story, in rural, north Idaho. My personal experiences
include every topic and every chapter in Breakdown,
supporting my daughter as best as I
can. My tenacious efforts have
partnered and often struggled with doctors, nurses, social workers, hospitals, living situations, guardianship proceedings, Social Security, Medicare,
Medicaid, the Department of Health and Welfare, law enforcement, Crisis Intervention
Team (CIT) police, and the National Alliance on Mental Illness (NAMI).
The complex mental
health system is far removed from Dorothea Dix’s advocacy efforts. But, how much
better off are people with serious mental illness, no longer shuttered away and
forgotten in insane asylums? Today medications replace straight jackets while
the Institutions for Mental
Diseases Exclusion law did away with 400-bed hospitals, which in turn
led to homelessness, violence, victimization, addictions, inadequate resources,
best-guess medication practices, revolving door social services, fatigued
families, and abandonment. What we have here is a multi-faceted “Problem Pile-Up.”
Geographic population densities
differ. Massachusetts has 839 people per square mile while Idaho has nineteen people per
square mile according to United States Census Quick Facts. A great source to
compare individual states is the Treatment Advocacy Center (TAC), which reports that in Massachusetts with a population of 5.5
million, 60,000 people live with schizophrenia. In Idaho with a population of
1.3 million, 14,000 people live with schizophrenia. The TAC statistics reference
United States Census statistics. Coincidentally, one percent of the population of
each of these states live with schizophrenia, which begs the question…where do
these facts originate? Are the solutions the same in both urban and rural
America?
While statistics and
anti-stigma campaigns are useful to start conversations, CIT may save lives,
NAMI classes educate family members, Mental Health Courts and Assertive
Community Treatment teams may restore some people to better lives, my humble
opinion is that these noble and worthwhile efforts are but band-aids on our
society which is bleeding out. No one sets out to be homeless, incarcerated,
hospitalized, die by suicide, or face an accidental early death. Policy makers need
the education to give priority to the people affected by serious mental
illness, the most difficult task. To be trite, an ounce of prevention is worth
a pound of cure. There is no one-size-fits-all solution. There is a giant
elephant in our living room and there isn’t a circus tent big enough to house
her ill body. Together, one bite at a time, with a dedicated commitment to
constancy, structure, encouragement, and acceptance, we can make changes that
would make Dorothea Dix proud.
I have yet to
personally meet authors Lynn Nanos, E. Fuller Torrey, Pete Earley, DJ Jaffe, Robert
Laitman and others. Their writings and advocacy work through books and social
media are enabling me to be a more knowledgeable advocate for my daughter and
other people who are so disabled that they can’t speak for themselves. I hope
that you will join our efforts!
Gini Woodward,
Mother of a fifty-year-old daughter with schizophrenia
Bachelor of Arts in Social Sciences
Past Experience:
NAMI Family-to-Family
Educator
NAMI family support
group facilitator
Idaho Region 1
Behavioral Health Board member and State Hospital
North Advisory Board member